Frequently Asked Questions
This FAQ is organized by topic to help you quickly find answers based on where you are in the process – whether you’re just starting to explore services, preparing to apply, or already receiving support. The structure follows a typical applicant’s journey: understanding eligibility, applying for services, finding providers, using available supports, and managing your benefits over time. This makes it easier to get the information you need, when you need it.
Eligibility & Definitions
This section clarifies the foundational concepts – what IDD is, who qualifies, and what programs like the iBudget Waiver and CDC+ are. It’s ideal for users new to the system or just starting their research.
What is IDD and who qualifies for services in Florida?
In Florida, IDD stands for Intellectual and Developmental Disabilities, and it refers to a range of conditions that affect a person’s intellectual and social development, impacting their ability to learn, adapt, and function in daily life.To qualify for IDD services in Florida, individuals must be Florida residents, aged 18 or older, meet specific eligibility requirements, and be diagnosed with a qualifying disability, as well as be eligible for Medicaid and reside in specific pilot regions.
What is the Florida Medicaid iBudget Waiver?
The Florida Medicaid iBudget Waiver is a home and community-based services waiver program for individuals with developmental disabilities. It allows eligible people to receive services in their homes or communities, promoting self-determination and preventing institutionalization. The program is managed by the Agency for Persons with Disabilities (APD) and funded through Medicaid.
What is the difference between the Florida iBudget Waiver and regular Medicaid?
iBudget is a Florida Medicaid Home and Community-Based Services (HCBS) waiver designed for individuals with developmental disabilities. Regular Medicaid, on the other hand, provides a broader range of medical services to a wider population. iBudget focuses on long-term care and supports for individuals with developmental disabilities, offering them more flexibility and choice in their care.
Detailed Breakdown
- Administration: Administered by the Agency for Persons with Disabilities (APD).
- Target Population: Individuals with developmental disabilities who meet specific criteria, including a need for the level of care typically provided in an intermediate care facility.
- Services: Focuses on services like supported living, supported employment, and other community-based supports to help individuals with disabilities live independently.
- Flexibility: Allows individuals more control over their care, including choosing providers and services that best meet their needs.
- Individual Budgeting: The “iBudget” name reflects a system where individuals are allocated a budget to spend on their supports and services, with flexibility to choose how to use those funds.
- Administration: Administered by the Florida Agency for Health Care Administration (AHCA).
- Target Population: A broad range of individuals, including low-income families, children, seniors, and individuals with disabilities.
- Services: Covers a wide array of medical services, including doctor visits, hospital care, prescription drugs, and mental health services.
- Flexibility: While regular Medicaid offers a range of benefits, it may not always provide the same level of flexibility and choice as iBudget, particularly regarding long-term care and supports.
Who is eligible for Consumer-Directed Care Plus (CDC+)?
In Florida, individuals are eligible for Consumer Directed Care Plus (CDC+) if they meet specific criteria, including being a current consumer under the Medicaid Waiver program, living in a family home or their own home, complete CDC+ training, and pass a Readiness Review test.
Video Introduction
Which IQ assessments are recognized by the Florida Agency for Persons with Disabilities as valid and reliable?
Standardized tests may be submitted as proof of an intellectual disability. The following are presumptively accepted standardized tests of intelligence to establish eligibility for an intellectual disability. The applicant must demonstrate that any test not presumptively accepted by the Agency is valid.
- Stanford-Binet Intelligence Test is a widely used, individually administered assessment that measures cognitive abilities across areas such as reasoning, memory, and problem-solving to produce an overall intelligence quotient (IQ). It is suitable for individuals aged 2 through adulthood and is often used for educational placement, diagnosis of intellectual or developmental disabilities, and eligibility for services.
- Wechsler Preschool and Primary Scale of Intelligence (WPPSI) is a standardized, individually administered test designed to assess the cognitive development of young children, typically ages 2 years 6 months to 7 years 7 months. It evaluates a child’s intellectual functioning across areas such as verbal comprehension, visual-spatial processing, working memory, and fluid reasoning. The WPPSI is commonly used for early educational planning, developmental assessments, and determining eligibility for special education or disability-related services.
- Differential Ability Scales – Preschool Edition (DAS-Preschool) is an individually administered cognitive assessment designed for children aged 2 years 6 months to 6 years 11 months. It measures a range of cognitive abilities including verbal and nonverbal reasoning, processing speed, and spatial abilities. The DAS-Preschool provides a General Conceptual Ability (GCA) score, which functions similarly to an IQ score. It is used to identify developmental strengths and weaknesses, support early intervention, and assist in determining eligibility for special education or disability services.
- Wechsler Intelligence Scale for Children (WISC) is an individually administered test designed to assess the cognitive abilities of children aged 6 to 15 years, 11 months. It evaluates areas such as verbal comprehension, visual-spatial skills, working memory, processing speed, and fluid reasoning to produce a Full-Scale IQ score.
- Differential Ability Scales (DAS) is a standardized test used to assess cognitive abilities, processing skills, and academic achievement in children from ages 2.5 to 15 years, 11 months. It helps identify learning strengths and weaknesses, often to support educational planning or diagnose developmental disorders.
- Wechsler Adult Intelligence Scale (WAIS) is a widely used test that measures adult intelligence through a series of verbal and non-verbal subtests. It assesses areas like memory, reasoning, comprehension, and processing speed to provide an overall IQ score and cognitive profile.
- Test of Nonverbal Intelligence (TONI) is a language-free assessment that measures general intelligence, problem-solving, and abstract reasoning using only visual and symbolic tasks. It’s especially useful for individuals with speech, language, or hearing impairments, or those from diverse linguistic backgrounds.
- Comprehensive Test of Nonverbal Intelligence (CTONI) evaluates general reasoning and problem-solving skills using nonverbal formats like pictures and geometric designs. It is designed for individuals ages 6 to 89, making it ideal for those with language, hearing, or cultural differences.
- Universal Nonverbal Intelligence Test (UNIT) is a completely nonverbal assessment of intelligence that uses gestures and visual tasks to evaluate memory and reasoning skills. It is designed for children and adolescents, particularly those who have speech, language, or hearing impairments, or are from culturally diverse backgrounds.
- Leiter International Performance Scale-Revised (Leiter-R) is a nonverbal intelligence and cognitive abilities test designed for individuals aged 2 to 20. It is ideal for those with speech, language, or hearing challenges, as it uses only visual and motor tasks without requiring verbal responses.
It’s important to note that APD requires assessments to be individually administered by qualified professionals authorized under Florida law. Additionally, beyond IQ assessments, APD requires evidence of significant limitations in adaptive functioning that manifested before the age of 18. This includes deficits in areas such as communication, self-care, and social skills.
Applying for Services
These FAQs guide you through the application process, including how to apply, wait times, and submitting a crisis request. It’s especially useful for those ready to take action or in urgent need of services.
How do I apply for the iBudget Medicaid Waiver?
To apply for the iBudget Medicaid Waiver in Florida, you need to submit an application to the Agency for Persons with Disabilities (APD) regional office where you reside. You can also apply online through the APD website. The iBudget Waiver is a Home and Community-Based Services (HCBS) waiver that provides individuals with developmental disabilities with flexibility to choose medically necessary services.
Detailed Breakdown of the Application Process
- Determine Eligibility:Ensure you meet the eligibility requirements for the iBudget Waiver, which include:
- Being a Florida resident.
- Having a diagnosis of a developmental disability.
- Meeting the level of care criteria for an Intermediate Care Facility for the Developmentally Disabled (ICF/IID).
- Being eligible for Medicaid.
- Gather Necessary Documents: You will need to provide documentation to support your application, including proof of residency, diagnosis, and financial information.
- Submit the Application: You can apply online through the APD website or by submitting a paper application to the APD regional office serving your area.
- Wait for Determination: The APD will review your application and determine if you are eligible for the iBudget Waiver.
- Enrollment: If approved, you will need to enroll in the iBudget Waiver program. This may involve signing a Medicaid Waiver Services Agreement (MWSA) with APD.
Additional Information:
- There is a waitlist for enrollment into the iBudget Waiver program.
- You may need to meet “crisis priority” to move off the waitlist.
- The APD provides resources and information about the iBudget Waiver on their website.
How long is the waitlist for the iBudget Waiver?
The waitlist for the iBudget Waiver in Florida can be very long, with some individuals waiting for years to receive services. In 2024, the average wait time was 40 months, according to a KFF report. The waitlist was first over 20,000 in May 2011, and as of January 2023, there were 22,372 people on the waitlist. While waiting, individuals may still be eligible for other types of Home and Community Based Services (HCBS).
How do I submit a Crisis Request from APD?
Individuals currently experiencing homelessness who exhibit life-threatening behaviors that pose an imminent risk to themselves or others, or who have a caregiver in extreme distress and unable to provide for their health and safety, may submit a request for crisis enrollment through the Agency for Persons with Disabilities (APD) iBudget Waiver program. Unlike the regular iBudget waiver process, there is no waitlist for crisis enrollment. This means that individuals in genuine crisis situations, such as those at immediate risk of harm, homelessness, or losing a caregiver, are not required to wait in line like others on the regular iBudget waiver waitlist. Instead, crisis cases are reviewed on a faster track to promptly intervene and prevent serious harm.
If you are in need of short-term emergency services, please contact your regional office serving your area or your Waiver Support Coordinator, if you have one. APD will review your situation to determine if a crisis waiver enrollment request is appropriate. To expedite your request, it is essential to thoroughly document the circumstances. Include relevant documentation such as doctor’s notes, Department of Children and Families (DCF) reports, eviction notices, police reports, or hospital discharges.
Upon receipt of your request, APD has 45 days to approve or deny the crisis enrollment. It is crucial to request a written response from APD in all cases. If your request is denied, you have the right to appeal the decision.
Coordinators, Providers, and Finding Help
This group helps you navigate the network of support, from finding a support coordinator to understanding the role of Family Care Councils and how to use 2-1-1 for local resources.
How Do I find a Waiver Support Coordinator in my Area?
To find a Waiver Support Coordinator (WSC) in your area, you can use the Agency for Persons with Disabilities (APD) Waiver Support Scorecard or the Florida Developmental Disabilities Resources website. Both resources allow you to search for WSCs by county or region.
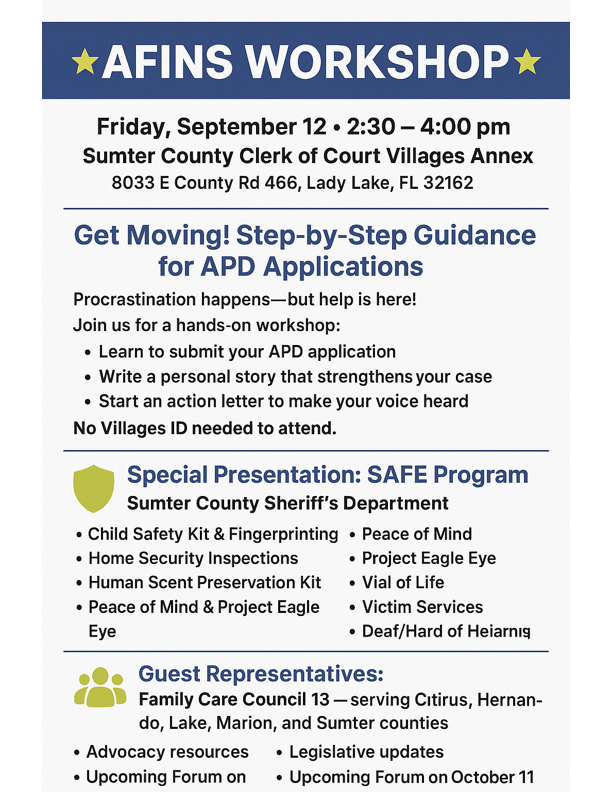
You can also contact your local APD Regional Office for personalized assistance or request a specific WSC. Alternatively, you can connect with other families and support groups, join Family Care Councils, Advancing Families and Individuals Needing Services (AFINS), or Facebook groups for personal recommendations.
How do I find an iBudget waiver service provider in my area?
To find iBudget waiver service providers in your area, you can use the Florida Developmental Disabilities Resources website and search by county or by APD region. You can also specify the type of service you need.
You can also contact your local APD Regional Office for personalized assistance or ask your Waiver Support Coordinator (WSC). They should have access to updated directories and availability information. Alternatively, you can connect with other families and support groups, join Family Care Councils, Advancing Families and Individuals Needing Services (AFINS), or Facebook groups for personal recommendations.
What are the Family Care Councils?
The Family Care Councils (FCC) in Florida are advisory groups made up of individuals with developmental disabilities and their family members. They work in partnership with the Agency for Persons with Disabilities (APD) to advocate for quality services, share information, and support individuals in making informed choices about their care. Each region in Florida has its own council that meets regularly to discuss local needs, promote inclusion, and provide feedback to APD on how to improve programs and services.
Getting involved is easy and meaningful. Anyone receiving APD services, or their family members or legal guardians, can attend meetings, participate in discussions, and even apply to become a council member. Membership applications are available through your regional Famly Care Council and must be approved by the Governor’s Office. Attending a meeting is a great first step, whether you’re looking to become a member or simply want to learn more. Visit the FCC website to learn more and click here to find your regional council and meeting schedule.
What is 2-1-1 phone service?
2-1-1 is a free, multilingual, confidential telephone service that supports community well-being. It provides information and referrals to non-emergency services, including assistance with housing, food, healthcare, employment, and more. 2-1-1 serves as a centralized resource for connecting individuals with appropriate assistance, and it is available 24/7/365. 2-1-1 facilitates access to local resources and services tailored to the specific needs of callers.
How to Use 2-1-1
- Call: Dial 211 on your phone.
- Visit the website: Search online for 211 in your area, or visit the United Way’s 211 website (www.211.org).
- Text: Text your zip code to 898-211 for assistance.
Services, Supports & Program Options
Here, you learn what services are available, how to use them, and what options like CDC+ and employment supports exist. It helps people already in the system or planning how to use their benefits.
What services and products are available through the iBudget Waiver?
The Florida iBudget Waiver provides a wide range of services and products to individuals with developmental disabilities, aimed at promoting independence and community living. These include assistance with daily living activities, therapeutic support, and specialized services like behavior analysis and mental health counseling.
Citation
What is Consumer-Directed Care Plus (CDC+)?
Consumer-Directed Care Plus (CDC+) is a Florida Medicaid program that allows individuals to directly manage their own long-term care services, including choosing their own providers and setting their own schedules. It’s an alternative to traditional Medicaid Home and Community-Based Services (HCBS) waivers, empowering participants to make decisions about their care and achieve their goals.
Key Features
- Choice and Control: Individuals have the flexibility to select their care providers, schedule services, and determine how their budget is spent.
- Self-Direction: Participants are expected to be involved in all aspects of planning their care, including choosing services, providers, and how they will be delivered.
- Flexibility: The program allows for more personalized support and services to meet individual needs and preferences.
- Increased Satisfaction: CDC+ participants report higher levels of satisfaction with their care and services.
- Independence: The program promotes greater self-determination and independence for individuals.
Video Introduction
Can I work and still receive services through the iBudget Waiver?
Yes, you can work and still receive services through the iBudget Waiver program in Florida. The iBudget Waiver is designed to help individuals with intellectual and developmental disabilities live and work in their own homes and communities.
What happens if I don’t use all allocated hours in my APD service plan?
If you don’t use all your allocated hours with the Florida Agency for Persons with Disabilities (APD) within your service plan period, the unused hours generally do not carry over to the next period. Providers should bill for all days an individual is present in the program up to a yearly maximum, and are expected to continue providing services even if the maximum is reached before the year’s end.
Detailed Breakdown of Allocated Hours Not Being Utilized
- Short-term: Unused hours do not accumulate and cannot be carried over to the next month.
- Long-term: Prolonged underutilization may result in a reduction of your budget or service authorization during the next support plan review. APD may assume that the full allocated hours are not necessary.
- Important Note: It is crucial to document instances where services were unable to be utilized due to staff shortages, illness, or other valid reasons. This documentation safeguards your future allocation.
Are CWIC & WIPA Counselors the Same?
Community Work Incentives Counselor (CWIC) and WIPA are not the same, but they are related. A CWIC is a specific type of benefits planner employed by a Work Incentives Planning and Assistance (WIPA) project. WIPA is the program that provides funding for these services.
Here’s a more detailed explanation:
- WIPA: The Work Incentives Planning and Assistance (WIPA) program is a Social Security Administration (SSA) initiative that provides free, in-depth benefits counseling to Social Security disability beneficiaries.
- CWIC: A Community Work Incentives Counselor (CWIC) is a professional, certified by the Virginia Commonwealth University National Training & Data Center, who works for a WIPA project. CWICs provide individualized counseling to beneficiaries about how working may affect their Social Security benefits, like SSI and SSDI, and other public benefits like Medicare and Medicaid.
Guardianship (Legal & Decision-Making)
This category provides information about legal guardianship – what it is, who can become a guardian, how guardians are appointed, and what responsibilities they hold. You’ll find answers to common questions about the rights of the individual under guardianship, the decision-making authority of guardians, and how to request changes or end a guardianship.
What is guardianship?
Guardianship is a legal process where a court appoints a person (the guardian) to make decisions for an individual (the ward) who is deemed unable to make some or all decisions for themselves due to disability, illness, or incapacity.
Guardianship is powerful and sometimes necessary, but it also takes away rights. Always weigh whether a less restrictive alternative could work before moving forward.
Citations
When is guardianship necessary?
Guardianship is considered only when less restrictive alternatives (like a power of attorney, health care surrogate, or supported decision-making agreement) aren’t enough to protect the person (ward). It’s meant to be a last resort.
What types of guardianship exist in Florida?
- Plenary Guardianship: Full authority over all rights and decisions.
- Limited Guardianship: Only covers specific rights the person cannot handle (e.g., medical or financial).
- Guardian Advocacy (Florida-specific): A simpler form of guardianship for adults with developmental disabilities that does not require declaring the person incapacitated.
What rights can be removed under guardianship?
Depending on the court’s ruling, rights can include:
- Right to decide where to live.
- Right to consent to medical treatment.
- Right to manage money or property.
- Right to marry or contract.
Courts are encouraged to keep as many rights as possible with the individual.
What is Guardian Advocacy and how is it different?
Guardian Advocacy is a streamlined process available in Florida for adults with developmental disabilities (like cerebral palsy, autism, Down syndrome, Prader-Willi, spina bifida, or intellectual disability). Unlike full guardianship, the person doesn’t need to be declared “incapacitated” – the court just assigns a guardian advocate for the areas where support is needed.
What are alternatives to guardianship?
These options may be less restrictive and still provide needed protection.
- Power of Attorney: A legal document that authorizes a designated individual to act on behalf of another person in specified or broad matters, such as finances or healthcare.
- Health Care Surrogate: An individual legally designated to make medical decisions on behalf of another person when that person is incapacitated or unable to communicate their preferences.
- Representative Payee for Social Security Benefits: An individual or organization appointed by the Social Security Administration to manage Social Security or Supplemental Security Income benefits on behalf of a beneficiary who cannot manage their own funds.
- Special Needs Trust: A legal arrangement that holds and manages assets for the benefit of a person with disabilities without affecting their eligibility for government benefits.
Who can serve as a guardian?
Any competent adult Florida resident, or certain family members who live out of state can serve as a legal guardian. Professional guardians are available if family isn’t an option. The court must approve all guardians.
How much does it cost to get guardianship or guardian advocacy?
Costs vary but often include:
- Filing fees (around $400).
- Attorney fees (can range from $1,500–$5,000+).
- Ongoing reporting costs (annual accountings and plans must be filed with the court).
Guardian Advocacy is usually less expensive than plenary guardianship because it’s a simpler process.
What are the ongoing responsibilities of a guardian?
Guardians must:
- File annual reports to the court.
- Make decisions in the best interest of the person.
- Keep finances separate and transparent.
- Get court approval for major decisions (like selling property or changing residence).
Does guardianship end?
Yes, guardianship can end if:
- The ward regains capacity.
- The guardian resigns or is removed.
- The ward passes away.
Appeals, Policy, and Redesign
This category is for those who want to understand their rights, options for appeals, and upcoming policy changes, like the iBudget Redesign. It’s critical for those who may face service denials or need to prepare for changes.
Can I appeal APD or iBudget Waiver decisions?
In Florida, if the Florida Agency for Persons with Disabilities (APD) denies a hearing request, the applicant has the right to appeal the decision within 30 days of the date of the Final Order. This appeal is filed with the appropriate District Court of Appeal. The Final Order will provide details about how to file the appeal. Additionally, if an applicant disagrees with an agency’s decision, they can request a hearing within 30 days of receiving written notice of the agency’s intended action. It’s important to submit paperwork promptly and document everything.
What’s changing with the iBudget Redesign?
The Florida iBudget program, a Medicaid waiver for individuals with developmental disabilities, is undergoing a redesign and expansion. This includes a broader service called “Personal Supports” that encompasses various existing supports. Additionally, there’s a shift towards a more needs-based assessment tool (NG-QSI) to replace the previous algorithm, aiming for more equitable resource allocation and flexibility. A significant change is the automatic assignment of iBudget recipients to a managed care plan under the Statewide Medicaid Managed Care (SMMC) program, starting in February 2025.
Key Changes
1. New Service – Personal Supports:
- The “Personal Supports” service is a broader umbrella that encompasses current services like personal care, companion care, in-home supports, and respite care.
- This allows for greater flexibility in the types of tasks a worker can perform for an individual.
2. New Assessment Tool – NG-QSI:
- The NG-QSI assessment tool is being implemented to replace the previous algorithm.
- It will collect functional, physical, behavioral, and demographic information to better understand individual needs and support requirements.
- This will help with budget predictability and service identification while maintaining the flexibility of the iBudget waiver.
- The NG-QSI will also assess natural support levels, including caregiver details and living situations.
- This change will require statutory and rule modifications.
3. Statewide Medicaid Managed Care (SMMC) Integration:
- Beginning in February 2025, all voluntary Medicaid recipients, including iBudget recipients, will be automatically assigned to a managed care plan by the Agency for Health Care Administration (AHCA).
- Recipients will receive a letter explaining this change.
- This shift aims to integrate iBudget recipients into the broader SMMC program.
4. Other Key Changes:
- The Agency for Persons with Disabilities (APD) is working to ensure that Adult Day Training (ADT) and Supported Employment services are compliant with the Home and Community-Based Settings (HCBS) Rule.
- Florida has until March 2023 to achieve compliance with these regulations.
- Disability Rights Florida and the Florida Agency for Health Care Administration (AHCA) have proposed significant language changes to the Medicaid Developmental Disabilities (“iBudget”) Waiver.
Financials & Legal
Focused on income, assets, and legal questions, this group addresses common concerns about how personal or family finances may impact eligibility.
What are asset limitations for Medicaid in Florida?
Long-Term Care Medicaid (Nursing Home / HCBS Waiver / iBudget Waiver)
- Single Applicant: $2,000 in countable assets.
- Married Couple (both applying): $3,000 combined.
- Married Couple (one applying): $2,000 for the applicant; up to $157,920 for the non-applicant spouse (Community Spouse Resource Allowance).
Exempt (Non-Countable) Assets
- Primary residence (if equity is below $730,000).
- One vehicle.
- Personal belongings and household items.
- Prepaid funeral and burial plans.
- Certain retirement accounts, if structured properly.
Important Considerations
- Asset Transfers: Transferring assets to qualify for Medicaid can trigger a penalty period, delaying eligibility.
- Income Limits: In addition to asset limits, Medicaid has income limits. For 2025, the income cap for long-term care Medicaid is $2,901 per month. If income exceeds this, a Qualified Income Trust may be necessary.
If I claim my adult disabled child as a dependent on federal taxes, will it affect their Medicaid eligibility?
The IRS and Medicaid use separate rules and processes, so you can claim your adult disabled child as a dependent without affecting their Medicaid eligibility in most cases. But be cautious with specific Medicaid waiver or long-term care programs – those may have unique financial rules, though they generally don’t factor in parents’ tax returns once the individual is an adult. It is recommended that you contact your local Medicaid office or a qualified benefits advisor for guidance tailored to your situation.
Here are some key points to remember:
- Medicaid Eligibility Is Based on Income and Assets: For adults, Medicaid eligibility is typically based on the individual’s own income and assets, not the parent’s, even if they are claimed as a dependent on taxes.
- Claiming as a Tax Dependent Is Allowed: You are allowed to claim your adult disabled child as a dependent if they meet IRS criteria (typically based on total income and needing your support). This does not count their Medicaid eligibility income as your income.
- Exceptions – Long-Term Care and Waiver Programs: Some specific Medicaid programs (like those for institutional care or home/community-based services) may consider household income differently. In rare cases, especially when applying for Medicaid through a waiver program, the financial eligibility rules may factor in parental income if the child is living at home and under a certain age – usually under 18. For adults, it typically does not apply.
- Supplemental Security Income (SSI): If your child receives SSI, that benefit often determines Medicaid eligibility automatically. SSI eligibility is based solely on the individual’s income and resources, not whether they’re a dependent on someone else’s taxes.
Does the Agency for Persons with Disabilities or Medicaid need parents’ income information?
Once your child turns 18, they are legally considered an adult for Medicaid purposes. Only their own income and assets are used to determine eligibility for Medicaid Waiver programs like the iBudget Waiver. Your income is not included in the evaluation.
Social Security
These FAQs point applicants to federal benefits that often intersect with Florida services, helping them understand and connect with Social Security programs.
What are all of the Social Security benefit programs?
There are ten main Social Security benefit programs:
- Social Security Disability Insurance (SSDI) – For individuals who have worked and paid Social Security taxes but are unable to work due to a disability.
- Supplemental Security Income (SSI) – For individuals with disabilities (or 65+) who have limited income and resources, regardless of work history.
- Retirement Benefits – For individuals who have worked and paid into Social Security, available starting at age 62 (with reduced benefits).
- Survivor Benefits – For family members (spouse, child, dependent parent) of a deceased worker, based on the worker’s earnings record.
- Dependent Benefits – For spouses or children of individuals receiving Social Security retirement or disability benefits.
- Disabled Adult Child (DAC) Benefits – For adults (18+) with disabilities who were disabled before age 22 and whose parent is receiving Social Security retirement or disability benefits, or is deceased.
- Medicare – Health insurance for people 65+ or under 65 with certain disabilities, often linked to SSDI eligibility.
- Special Benefits for Noncitizens – For noncitizens who have worked in the U.S. and meet specific residency or work conditions.
- Workers’ Compensation Offset – For individuals who receive both SSDI and workers’ compensation benefits; SSDI may be reduced to avoid “double-dipping.”
- State-Supplemented SSI – Additional financial support for SSI recipients in some states to help with living expenses.
How do I contact the Social Security Administration?
The Social Security website, www.ssa.gov, is the best way to get help. If you cannot use their website, please call their National 800 Number (800-772-1213), or visit your local Social Security office. They can often help by phone and save you a trip to an office. If you need in-person help, you must make an appointment to visit a local office.
- Lake County: 900 N 14th Street, Leesburg FL, 34748, Suite 100
- Marion County: 933 E Silver Springs Blvd., Ocala FL, 34470
- Sumter County residents should visit either the local Lake or Marion County office.
Offices are busiest Mondays, the morning after a federal holiday, and the first week of the month.
Having a my Social Security account offers significant convenience and control over your Social Security information and benefits. It allows you to access your earnings record, estimate future benefits, change your address, and request a replacement Social Security card, among other things.
Other Key Contacts
This simple but essential category is for those who need to contact related agencies, like the Department of Children and Families, ensuring users know where to go next.
How do I contact Department of Children and Families?
- By Phone: Call DCF customer call center at (850) 300-4323.
- Online: Start at the DCF home page, or go directly to the their MyACCESS portal to start the application process. You can also schedule an appointment or get an e-ticket on their Online Ticketing System.
- Visit a Family Resource Center: Go to the DCF Family Resource Centers webpage to locate a facility by facility name, city, county or zip code.
You may do the following at the Family Resource Center without an appointment:
- Drop off any documentation
- Provide ID for authentication
- Use a computer to apply for government assistance
- Receive Department forms
All other services are by appointment only. Click here to make an appointment.
What are the 10 most frequently asked questions about the Americans with Disabilities Act (ADA)?
How do I apply for a caregiver guest ID in The Villages?
To obtain a Caregiver Guest ID in The Villages, the resident and caregiver must visit a District Customer Service Center together with the required documents: the resident’s Villages ID, the caregiver’s driver’s license and business license, and completed (but unsigned) copies of the Caregiver Guest ID Application and Contract for Services. At the center, they present the paperwork to the clerk and then sign both forms in the clerk’s presence.
You can download The Villages Caregiver Guest ID Package here. The package includes full instructions along with fillable PDF versions of the Caregiver Guest ID Application and the Contract for Services.