on January 31, 2020. the federal government declared a public health emergency for the COVID-19 pandemic. As a requirement to continue to receive additional funding from the federal government Florida has provided continuous Medicaid coverage to ensure healthcare continuity and has not unenrolled recipients whose household situation would make them no longer eligible. Florida saw a significant increase in the number of individuals and families seeking Medicaid assistance, from 3.8 million enrolled in March 2020 to 5.5 million in November 2022.
Since the continuous healthcare coverage provision ended on March 31, 2023 the Florida Department of Children and Families (DCF) has been reviewing Medicare cases to ensure recipients are eligible for benefits. DCF is trying to do this exercise quickly and fairly by prioritizing exceptional customer service through strong communication and community collaboration, and by leveraging technology solutions to enhance operational efficiencies while being compliant with federal guidelines.
Many individuals will be automatically reviewed and approved to continue Medicaid eligibility. In this case, they will receive a notice that their Medicaid case has been approved and their Medicaid coverage will continue. There is nothing more for them to do.
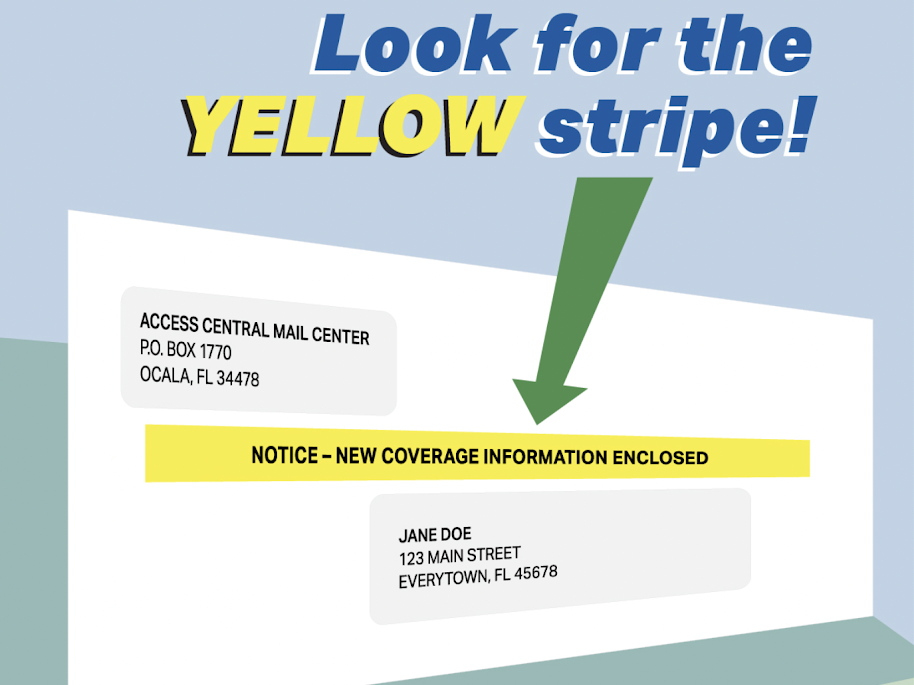
If DCF cannot automatically renew an individual’s Medicaid coverage because additional information is required, they will send a notice 45 days prior to the recipient’s renewal date with instructions on how to complete the renewal process. Individuals receiving such notices are given the opportunity to provide updated information to DCF. If you receive this notice, it is important to act timely and provide the requested information so that you do not experience any disruption in your Medicaid coverage.
The most prudent and quickest way to provide most updated information is to proactively log into your MyAccess account and update your case. If you need to provide documentation that cannot be entered into your MyAccess account, it is best to hand deliver it to the local DCF office. Make sure you get a date and time stamped receipt of delivery before leaving. If you must mail the information, use the United States Post Office Registered Mail service so that you have a receipt. Having a receipt proves that you provided the requested information if DCF misplaces it.
If it is determined that a Medicare recipient is no longer eligible and continuous coverage ends, they will receive notice from DCF. Individuals deemed ineligible for Medicaid, but eligible for a different healthcare coverage program, will automatically be referred to Florida KidCare, the Medically Needy Program, the Federal Marketplace, and other subsidized federal healthcare programs to ensure continuous healthcare coverage.
Florida KidCare provides low-cost health coverage for children based on family income. You can learn more about this program on their website. The Medically Needy Program allows Medicaid coverage after a monthly “share of cost” is met, determined by household size and family income. You can learn more about the Medically Needy program by downloading the Medically Needy Brochure.
If an individual’s application is transferred to the Federal Marketplace, they will receive a letter from the United States Department of Health and Human Services with instruction on how to complete an application for healthcare insurance. You can learn more about the Federal Marketplace at healthcare.gov.
If you have questions regarding your MyACCESS account, or about updating your contact information, please check out the Access Florida – Florida Department of Children and Families ‘How To’ videos.